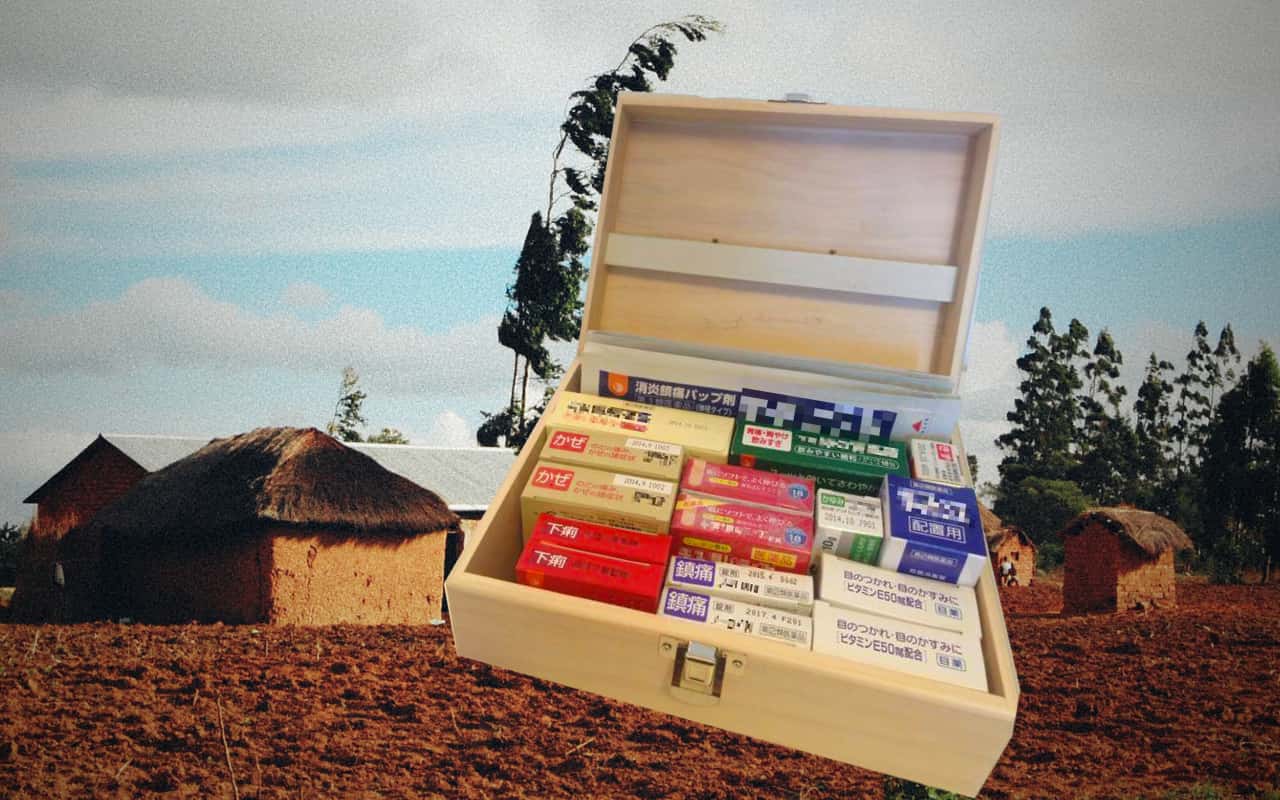
Bwama village is one of the world’s more remote places. Nearly inaccessible by road from Tanzania’s largest city, Dar es Salaam, during the long East African rainy season, the tiny hamlet lacks running water, sewage or electricity. Japanese consumer electronics — popular elsewhere in Africa — are in short supply here. But there is one surprising Japanese export that has found a niche: okigusuri, a centuries-old method of selling household medicine. Once ubiquitous in Japan, okigusuri has all but disappeared in the country that pioneered it.
Okigusuri is a compound of oku (to place) and kusuri (medicine). Popularized more than 300 years ago during the Edo Period, it is a “use first, pay later” system for selling basic medications—traditional kanpo (Chinese medicine) remedies back in the day; aspirin, diarrhea medicine and the like today. Users who sign up with an okigusuri service receive a box filled with drugs. A salesperson visits periodically to replenish the box and charge for the medicine that has been used since the last visit. The system was pioneered in Toyama and spread from there throughout Japan, but in modern times okigusuri has largely lost its place in Japanese society.1Ministry of Health, Labour and Welfare reports: 2007, 2017
Eri Machii decided to give okigusuri a second life in Africa.
A pharmacist by profession, Machii worked as a volunteer in Niger with the Japan International Cooperation Agency (JICA). Conditions in remote African communities, she noted, were similar in some ways to those of Edo period Japan. Lack of infrastructure makes it difficult for people to reach hospitals and clinics — and forget about popping out to a convenience store for over-the-counter remedies. Families are large and universal health care is not available.
Remote African communities face challenges that are similar in some ways to those of Edo Japan
In 2014, Machii established AfriMedico, a non-profit organization (NPO), along with a group of fellow pharmacists. By last year the organization had placed okigusuri boxes in more than 200 Tanzanian households.
AfriMedico’s version of okigusuri combines tradition and technology. With help from IT companies, the company uses sensors and artificial intelligence to keep track of customers’ medicine use. Local staff snap pictures of the boxes with smartphones and upload them to a server; an algorithm does the rest. The use of AI has increased accuracy by a third, Machii says.
Scientific evaluation of the efficacy of okigusuri in Tanzania awaits further statistical review, but Machii is gaining confidence in her project at the grassroots level. Villagers take comfort in having medicine close to hand, she says. Newsweek selected Machii as one of its “World’s 100 Most Respected Japanese People.”
Machii wants to use the trust that AfriMedico has built in places like Bwama to tackle broader healthcare problems, beginning with educating people about preventing illness. “Even if we bring in okigusuri, if we can’t stop villagers from drinking dirty water, for instance, our project will end up as a futile cat-and-mouse game,” she said.
AfriMedico combines tradition and technology, using sensors and artificial intelligence to track medicine use
In Niger, Machii taught local villagers how malaria occurs and how it can be prevented, but realized that far more work would be required to get them to make lasting lifestyle changes based on this knowledge. To fill in this gap, AfriMedico is developing a bottom-up educational program with local okigusuri managers.
Despite its initial success, AfriMedico is confronted by the limitations of being a small NPO. The 40 people who support the project in Japan all do so alongside full-time jobs. Fundraising has been fitful, preventing the project from progressing at a faster pace. Machii hopes that ongoing research into the effectiveness of the okigusuriproject, which AfriMedico is conducting in collaboration with a Tanzanian university, will help persuade the Tanzanian government to invest.
In the long run, Machii hopes to spread okigusuri to other parts of Africa where access to healthcare is limited. She aspires to develop a hub in west Africa and ultimately bring okigusuri to Niger — the place where she was first inspired to establish AfriMedico.
Another goal of AfriMedico is to connect Japan and Africa. As a part of this effort, the NPO has been working with the Tanzanian government and pharmaceutical companies to increase the number of approved Japanese medicines in Tanzania.
Rural depopulation could make a modernized version of okigusuri relevant once more in Japan
Machii thinks the spread of okigusuri in Africa might even spur innovation in the dying okigusuri industry in Japan, where rural depopulation is placing new kinds of pressure on healthcare infrastructure. Increasingly, isolated Japanese villages lack sufficient inhabitants to support a full-sized pharmacy.
“If we bring back the modernized version of the system developed in Africa, we could potentially revitalize the okigusuri industry in Japan,” Machii explained.
In overcoming the technical challenges required to bring this Japanese tradition to remote parts of Africa, she may have found a way to make it relevant once again in its country of origin.

This article was produced based on a series of events organized by Asia Pacific Initiative as part of the “Reinventing Japan” project. All opinions expressed are the author’s own and do not reflect the institutional position of Asia Pacific Initiative.
This piece was based on a presentation followed by discussion by Ms. Eri Machii, founder of AfriMedico.
Kenta Sayama is currently an intern at the UNHCR Representation in Japan, and was formerly an intern for the environmental protection agency in Manaus, Brazil. He recently completed his studies at Washington and Lee University in Virginia, USA, and is preparing to start a Masters degree at the University of Oxford.


















You must be logged in to post a comment.